 | 15 min read
| 15 min read
In this article I have summarized the different treatments that are available for acne scarring, explained how certain methods are more appropriate for some scar types and discussed my approach to combining these treatments.
The skin is composed of a thin outer barrier - the epidermis - and a deeper, thicker layer known as the dermis that gives strength and elasticity to the skin. Superficial acne lesions such as whiteheads and small inflammatory papules (spots) do not usually result in visible scars (although they can cause pigmentary change). In contrast, larger acne lesions - particularly cysts and nodules can cause significant damage to the dermis with infiltration of white blood cells. This tissue damage triggers the wound healing process which ultimately leads to the formation of a scar.
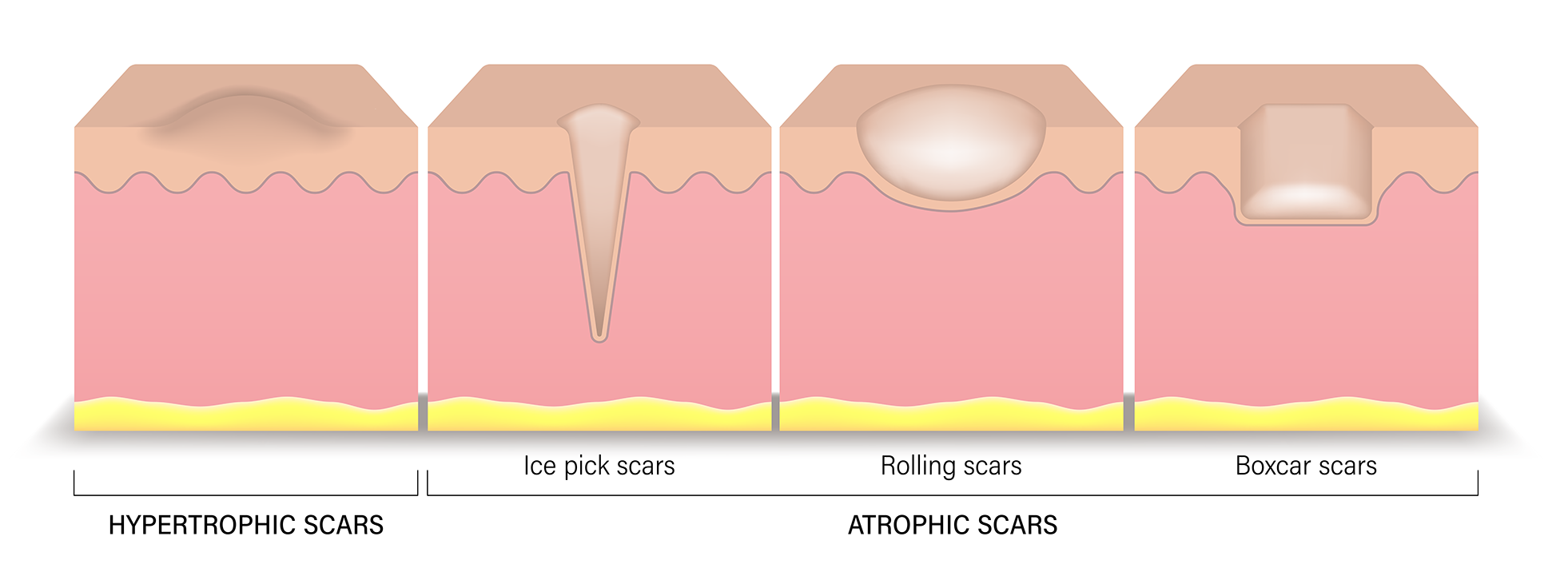
When acne scars are flush with the surface and similar in color to neighbouring skin they may be barely noticeable, however scar formation can result in loss of dermal volume resulting in depressed "atrophic" scars. Less commonly scars may be raised above the surface of the skin "hypertrophic" or "keloid" scars. Another reason why acne scars may be noticeable is when scars are different in color (lighter, darker or redder) in comparison to normal skin.
The best method for preventing scar formation is early and effective treatment of acne - with tablet treatments if necessary. This is particularly important for moderate-severe acne, especially where this is associated with cysts and nodules.

Atrophic (depressed) scars are classified according to the shape of the scar. This in turn will reflect the size and shape of the damage that was caused by the acne lesion in combination with how the healing process has progressed.
It is important to emphasize that in reality scars will not always fall neatly into one category and patients will typically have multiple different types of scars which often merge and overlap.
Treatments for atrophic scars are discussed in more detail below.
Tretinoin, a topical retinoid, promotes cell turnover and collagen production. This can help to gradually fade scars. It can be helpful for post-inflammatory hyperpigmentation and mild atrophic scars. However it is not effective for deeper scars.
Scarring caused by deep nodules and cysts can lead to the formation of fibrous bands which tether the skin to deeper tissues. This can exacerbate the dipped appearance and is particularly associated with rolling scars. Subcision is a procedure that will divide these fibrous bands.
Subcision is generally performed with a sharp-edged (Nokor) needle which is inserted under local anaesthetic through the skin surface and then manipulated to divide fibrous bands beneath the skin surface. Complications include bruising, infection and cyst formation.
Very rarely, where bruising is extensive it may need to be drained surgically, however a small amount of bruising is actually desirable since this reflects the presence of blood clot beneath the skin surface which can help to restore volume. Bruising typically lasts for 1-2 weeks after the procedure.
Subcision is a particularly effective treatment for tethered rolling scars and some other atrophic scars and generally I would advise that this is performed before other treatment methodologies.
Trichloroacetic (TCA) acid is a chemical which causes inflammation when applied to the surface of the skin. TCA CROSS stands for TCA chemical reconstruction of skin scars. This involves the precise application of small amounts of TCA to the base of atrophic (depressed) acne scars. This triggers the wound healing response which can lead to the depressed scar filling out and becoming less noticeable.
TCA CROSS is used for atrophic acne scars such as boxcar and rolling scars. In most cases more than one treatment is required.
Multiple areas can be treated in a single session. Following treatment the area will be red and sore for 5-7 days. You should apply Vaseline regularly until the treated areas have healed. Risks include persistent redness, increased pigmentation (post-inflammatory hyperpigmentation) and decreased pigmentation (hypopigmentation). Pigmentary change is more of a concern in those with darker skin types. It usually resolves spontaneously with time but very rarely can be permanent.
Where patients have a relatively small number of small, deep scars (usually ice pick scars) these can be be removed surgically using a punch device. A small, round core of skin is removed under local anaesthetic and one or more stitches are applied. This heals to give a straight line scar which is usually less noticeable. This can be an excellent treatment where there are a few deep scars, however it is less feasible when there is a large number of scars. Similarly, if there is a very localized area of severe scarring elliptical excision (cutting and stitching) can be an option.
A similar technique is punch elevation - here the punch tool is used to release a circle of skin at the base of the scar and this is then elevated to the level of the skin surface using carefully placed sutures.
Loss of dermal tissue volume is a particular challenge in treating acne scars. Smaller depressed scars can can be improved with TCA cross or punch excision, however where there are larger areas of volume loss these methods may not be sufficient. Dermal fillers can be of benefit for these scars. It is important to use a filler material that is pliant since this filler is placed in a superficial location and firmer fillers can lead to the appearance of nodules beneath the skin surface. Limitations of dermal fillers are that they are temporary and may need to be repeated.
Risks include over correction - leading to a raised rather than a depressed scar. Additionally there is a risk that the filler material can track to the outside of the scar causing a 'doughnut' appearance. For this reason I will always use hyaluronic acid-based fillers, which are temporary and can be dissolved though the injection of hyaluronidase.
Fractional laser resurfacing causes thousands of microscopic columns of precisely controlled injury within the dermis. This induces a healing process which leads to the formation of new collagen and can improve the appearance of superficial pitted acne scars and fine lines and wrinkles.
Fractional laser resurfacing cannot correct deeper areas of volume loss and I advise that more significant contour deformities are addressed first with subcision, punch excision or TCA cross.
Fractional lasers can be broadly divided into non-ablative lasers and ablative lasers. Non-ablative lasers, such as the erbium glass (ICON) laser cause selective damage to the dermis. This is associated with some redness and swelling for a few days following the procedure, however there is generally not blistering, crusting or shedding of the skin and the risk of pigmentary change is low. Non-ablative lasers usually require a course of several treatments.
Ablative laser, such as the carbon dioxide laser, cause damage to both the dermis and epidermis. This greater degree of damage leads to greater stimulation of wound healing response and can generate more collagen potentially allowing correction of more significant scars. The healing process takes substantially longer than for non-ablative lasers and is associated with redness, swelling, blistering and crusting. Additional risks include bacterial or viral (herpetic) infection and pigmentary change. 1-2 treatments can often lead to a substantial improvement. Due to the increased risks of this laser I will always advise that a small "test" patch is treated first to assess the healing.
The choice of which laser to use will depend upon the nature of your scarring, your skin type and the degree of risk and downtime that you are willing to accept. I will discuss the advantages and disadvantages with you at the time of your consultation.
Scars that are raised above the level of the skin surface are known as hypertrophic. When scars spread beyond the site of the original acne lesion these are keloid scars. Certain individuals have a tendency to form this type of scar and there is a risk that they can recur despite treatment.
Treatment of hypertrophic and keloid scars is challenging because certain individuals have a tendency to the formation of this type of scar and any interventional procedure or laser treatment carries the risk of triggering new scar formation or worsening existing scarring. Generally I will use cautious injection of steroid in this context.
Even when they are flush with the skin surface, Acne scars may be noticeable because they are different in color compared to the normal skin color.
Redness of the scar is known as "post-inflammatory erythema" (PIE). It is caused by an increased number of blood vessels in the scar tissue compared to the normal skin. Some degree of redness is normal in the early phase of healing and for most scars will fade spontaneously with time, however occasionally this will persist and can make the scars stand out.
Redness is common in the early phase of acne scar healing and generally will resolve with time. This is known as post inflammatory erythema (PIE). It reflects an increased number of blood vessels present at the skin surface as part of the natural healing process.
For some patients this redness can persist after the scar has healed. This can be treated with the pulsed dye laser.
Darkness of the scar is known as "post-inflammatory hyperpigmentation" (PIH). This is much more common in those with pigmented skin types. It is caused by increased production of pigment due to inflammation in addition to damage to pigment-producing cells "melanocytes" that causes them to 'fall' from the surface of the dermis to deeper locations where they can persist for many months or years. Whilst it will improve with time topical and laser (Q switched or pico laser) can be helpful.
Acne scars can also be lighter in color than the normal skin type "hypopigmented". This is less common than redder or darker scars and is much more noticeable in those with pigmented skin types. Treatment is challenging - fractional laser resurfacing, topical prostaglandins and melanocyte transplantation have been tried with variable success.
Generally it is advisable to address the most significant contour deformities first. If there are tethered scars I will advise subcision as the first stage of treatment. This can be followed by TCA cross and/or punch excision if required either on the same visit or subsequently. Once the major contour deformities have been addressed we can then consider fractional laser resurfacing to address more superficial pitted scars and any irregularities resulting from these previous procedures.
Acne scarring is one of the most challenging conditions treated by the dermatological surgeon. Treatments must be tailored to the types of scarring that are present, your skin type and the degree of downtime and risk that is acceptable to you. Nevertheless, significant improvements can be achieved.
If you would like to explore potential treatment options for acne scarring, please contact my practice management team to schedule a consultation. In person consultations are preferred to remote as I can better assess the 3-dimensional morphology of scars and check for tethering of scars to deeper structures.
To book an in person consultation, enter your details below and my practice management team will contact you to schedule the appointment. Alternatively call 0203 389 6076 (calls are answered during working hours) or email: contact@drmagnuslynch.com.